|
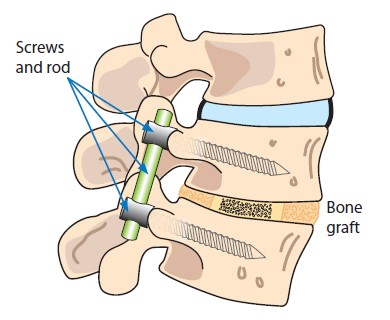
Surgery involves using metal implants which are attached to the spine and then connected to rods. The metalwork is used to correct the position of the spine and hold it in to the corrected position until the spinal segments fuse together. Fragments of bone are placed along the length of the corrected spine stimulating healing essential to maintain the spine in the corrected position.
The surgery can be performed from the back of the spine (posterior approach), through a straight incision along the midline of the back or through the front of the spine (anterior approach), through the side of the chest, or a combination of both anterior and posterior approaches.
|
|
Drains may be inserted during surgery to drain any excess blood that may collect post operatively. Drains will be removed between 24-48 hours post operatively.
The fusions within the spine harden in a straightened position to prevent further curvature, leaving the rest of the spine flexible. It takes about 3 months for the vertebrae to fuse substantially, although 1-2 years are required before fusion is complete.
|
|
-
Pain. Pain or soreness in ADDITION to the discomfort experienced after surgery that can be long-lasting.
-
Delayed healing of wound.
-
Nerve damage. This is damage to the spinal nerves which can cause weakness, pins and needles, temperature change or reduced feeling in your legs. At worst this can be complete paralysis.
-
Eyesight damage. Very rarely patients can report damage to their eyesight.
-
Failure of the metalwork. Rarely the rods or screws used to correct the spine can break or become detached from the spine often because the spine has failed to heal properly.
-
Further surgery. A number of patients will require further surgery to address curves that persist following surgery or to treat complications that have arisen.
|
|
-
Constipation. Some analgesics can cause constipation; daily walking, fibre rich diet and oral laxatives can help. It is important to regain your normal bowel habit to avoid straining.
-
Deep vein thrombosis (DVT). You will be asked to wear compression stockings post operatively and may have electronic flowtron boots which compress your calf to prevent DVT. There is a risk of developing a blood clot in your leg as you have reduced mobility for a short period of time during and after the operation. You should regularly move your legs and wiggle your toes to encourage good circulation, especially when in bed. Early mobility is encouraged.
|
|
Smoking. It is important that you stop smoking. Smoking has been shown to increase complications after major surgery, increasing risk of chest infection. Smoking may also effect the healing of the metal work and fusion of the spine.
If any of these complications happen once discharged please contact:
Kelly Jackson
Enhanced Recovery after Surgery Specialist Nurse
 0161 206 0194 0161 206 0194
Email:
 kelly.jackson@srft.nhs.uk kelly.jackson@srft.nhs.uk
|
|
You may experience discomfort in your back and hips from spending time in one position and your wound may be painful. These are all consequences of the surgery you have had and will disappear over time.
You may experience some pain in the area where you had the operation. You will wake up with a catheter in and once you start to mobilise this will be removed. It is normal to be in some discomfort but let the nurse know if your pain stops you from doing normal things like eating, sleeping, walking and going to the toilet.
Whilst in hospital the nurse will check on you regularly to give appropriate pain relief. Following your surgery a nurse will assist you to get out of bed and walk to the bathroom. The nursing staff will redress your wound; you are advised not to shower or bath for the first 10 days.
|
|
Post-surgery you will be seen by a physiotherapist who will assess your strength, mobility, balance and encourage walking. Please see post-op advice booklet (in PDF format bellow) for specific details.
Occasionally the consultant may suggest a brace post operatively; if this is appropriate for you, you will be provided with more information. An orthotist will supply a brace and help you fit the brace initially. You will need to be independent with placing this on and off and understand when to wear the brace before going home. You may need someone at home to be able to put the brace on correctly.
The physiotherapist will practice stairs with you prior to discharge and you will need to be independently mobile with or without an aid to be ready for home. Usually, young people do not normally require ongoing physiotherapy once you are discharged from hospital.
|
|
Length of stay in hospital may vary and will depend on a number of factors:
An outpatient clinic appointment will be made for you to see the specialist spinal nurse in clinic usually 6 weeks post op. You will be reviewed in consultant clinic approximately 3 months post-surgery. An appointment will be sent to your home.
|